Swiss ophthalmology practices are facing growing pressure. An aging population, an increase in chronic eye diseases, and a shortage of specialists… The volume of requests is growing faster than the capacity for care.
In this context, continuing to operate on a “first come, first served” basis quickly reaches its limits. This is precisely where triage in ophthalmology becomes a key lever. When well structured, it allows you to prioritize patients who need it most, while improving patient flow and the daily lives of staff.
What is meant by triage in ophthalmology?
As in other specialties, triage in ophthalmology involves quickly assessing the severity of a clinical situation to determine the most appropriate time for care. It’s not about making a final diagnosis, but about ranking requests based on the risk to the patient’s vision and the potential urgency.
To do so, you must consider:
- The symptoms described by the patient
- Their onset
- Their progression
- The presence or absence of pain
- The general medical context
Why structuring triage has become essential in ophthalmology practices
In many practices, triage still largely relies on individual experience, intuition, or the “first come, first served” approach mentioned in the introduction. While this may work on a small scale, it quickly shows its limits as soon as the volume of calls and requests increases.
Unstructured triage exposes you to several risks:
- Delays in patient care
- Disruption of the appointment schedule
- Overload of the front desk
- A loss of control felt by teams
By directing patients more effectively, you save time and can focus on situations with higher clinical value.
The three levels of triage in ophthalmology
Most ophthalmology practices rely on a simple three-level classification, such as the Rome Eye System for Scoring Urgency and Emergency (RESCUE). These three levels are often paired with a color code (red, orange, yellow). This method has the advantage of being easy to understand and quick to apply, especially for administrative staff.
Its main limitation, however, is subjectivity if the criteria are not clearly defined. Without a precise framework, two people may classify the same situation differently.
| Category | Description | Recommended timeframe |
|---|---|---|
| Emergency (red) | Situation directly threatening vision | Immediate / within a few hours |
| Urgent (orange) | Potential short-term risk | 24 to 48 hours |
| Non-urgent (yellow) | Stable situation | Several days to weeks |
Ophthalmic emergencies (immediate care)
Certain situations must be identified without delay, as they directly affect visual prognosis. Among the most frequent warning signs are:
- Sudden and persistent vision loss
- Severe eye pain
- A painful red eye
- A recent eye trauma
Suspected retinal detachment, the presence of an intraocular foreign body, or chemical burns also require immediate action. Finally, associated neurological symptoms (speech disorders, motor deficits, severe headaches) should prompt urgent care outside the practice.
Urgent situations (care within 24 to 48 hours)
Other situations, while not immediately sight-threatening, require rapid assessment. This includes, for example:
- Recent-onset diplopia
- Distorted vision
- Redness accompanied by discharge
- Persistent blurred vision without pain.
Situations not requiring immediate care
Some situations may be uncomfortable for the patient but do not pose a short-term risk to vision. These cases can easily be managed at a later stage once emergencies have been addressed.
Triage methods used by high-performing ophthalmology practices
The most efficient ophthalmology practices share one thing in common: triage is neither improvised nor left to chance, but relies on clear methods adapted to real-world practice. The goal is not to complicate processes, but rather to gain speed and consistency in decision-making.
More advanced and customised scoring systems
It is recommended to customise classifications to your practice and your on-the-ground expertise. This saves time on documentation and improves efficiency when sorting patients.
In practice, this can take the form of a simplified scoring grid used by the team during first contact. For example, some practices assign points based on a few key criteria: sudden onset of symptoms, presence of pain, objectively reduced vision, or a traumatic context. A high score automatically triggers a rapid consultation, while a low score leads to a longer timeframe or simple advice.
This pragmatic approach, inspired by models such as RESCUE but adapted locally, helps standardise decisions without excessive rigidity.
Link with referring physicians
Effective triage does not stop at the practice door. The best centres work closely with referring physicians. Collaborating with trusted partners who regularly refer patients makes organisation easier. A solid understanding of their practices helps anticipate requests and orient patients more quickly according to the severity of their condition. This coordination improves prioritisation and makes the care pathway smoother.
When necessary, you can also refer patients whose situation does not require immediate specialist care to a general practitioner or another more appropriate professional.
This mutual understanding helps anticipate demand, reduce inappropriate consultations, and more quickly direct truly high-priority patients.
Continuous improvement based on feedback
No triage system is perfect. The most high-performing ophthalmology practices are those that take the time to regularly analyse past decisions.
Reviewing an underestimated case—or, conversely, one that was over-prioritised—helps identify signals that were missed or overinterpreted. These experiences can be shared during team meetings, where criteria are adjusted and practices harmonised. This collective dynamic embeds triage in a continuous improvement mindset, benefiting both patients and teams.
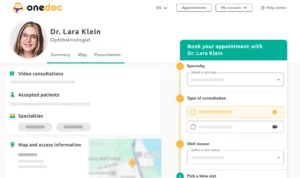
Remote triage and pre-triage in modern practice organisation
The evolution of medical practice is leading more and more clinics to integrate pre-triage into their organisation. By collecting certain information before the appointment, it becomes possible to better qualify requests from the very first contact.
Several studies show that remote triage, particularly in a tele-ophthalmology setting, can improve the relevance of prioritisation. In just a few minutes, you can assess the patient’s condition and pre-categorise it according to your practice’s triage grid, or advise them to stay at home if consultation is not required.
AI as an aid to triage
Artificial intelligence also opens up new perspectives. A study published in Digital Health showed that a properly trained chatbot could perform initial patient triage with results comparable to those of ophthalmologists.
Used as a support tool, this technology can facilitate structured symptom collection, reduce administrative burden, and more effectively guide patients. The goal is not to replace medical expertise, but to free up time so that you and your team can focus on care requiring your expertise.
Towards more efficient ophthalmic triage
In a context of growing pressure on ophthalmic care, structuring triage has become a necessity. By applying these best practices, triage can become a true strategic lever, allowing you to free up time for ophthalmic care.
Source
- AlSamnan, M., AlAmry, M., Aldossari, S., Talea, M., Khandekar, R., & AlGhadeer, H. (2023). Validity of an Ocular Emergency Triage System Compared to the Existing Grading System at the Emergency Unit of a Tertiary Eye Hospital in Saudi Arabia. Clinical ophthalmology (Auckland, N.Z.), 17, 527–534. https://doi.org/10.2147/OPTH.S397504.
- Jost, A. Build a successful triage team, Ophthalmic Professional.
- Optometry-evolution: Mastering Emergency Eye Care: Essential Triage Guidelines for Eye Conditions.
- Rossi T, Boccassini B, Iossa M, Mutolo MG, Lesnoni G, Mutolo PA. Triaging and Coding Ophthalmic Emergency – the Rome Eye Scoring System for Urgency and Emergency (RESCUE): A Pilot Study of 1000 Eye-Dedicated Emergency Room Patients. European Journal of Ophthalmology. 2018;17(3):413-417. doi:10.1177/112067210701700324.
- Schumacher, I., Ferro Desideri, L., Bühler, V. M. M., Sagurski, N., Subhi, Y., Bhardwaj, G., Roth, J., & Anguita, R. (2025). Performance analysis of an emergency triage system in ophthalmology using a customized CHATBOT. Digital health, 11, 20552076251320298. doi:10.1177/20552076251320298.
- Solís, Rafael & Griñolo, Mª & Zúñiga, Beatriz & Albert, Beatriz & Villar, María & Troncoso, María & Pablos, Rocío & Franch, Enrique. (2025). Effective Validation of Primary Care Patient Triage Classification Via Tele-Ophthalmology With Optometrist Support. INQUIRY: The Journal of Health Care Organization, Provision, and Financing. 62. 10.1177/00469580251367231.