Healthcare professionals in Switzerland see it every day: more patients, more chronic diseases and… more administrative work. In a historically fragmented care network, information is difficult to share, patient pathways lack fluidity and follow‑up becomes more complex. Today, the question is no longer just about improving care, but about building a true health network capable of anticipating, preventing and coordinating better. Discover in this article the challenges of the current healthcare system in Switzerland and the solutions that can support this transition toward a health network.
1. Care network vs health network: what is the situation in Switzerland?
1.1 The care network: coordination around the patient
Traditionally, a care network refers to all the professionals involved in a patient’s care: primary care doctors, specialists, nurses, physiotherapists, psychologists, nursing homes, hospitals, pharmacies, social services, etc. In Switzerland, this network is historically highly fragmented: cantonal structures, multiple insurers, numerous private and public actors… All of this complicates coordination and continuity of care. Care becomes complex and pathways difficult for patients to understand. Under pressure in the health system, this fragmentation has reached its limits. The National Research Programme “Health System” (PNR 74) of the SNSF highlights the importance of better coordinating the many professionals involved, involving patients’ support networks more and developing new interprofessional care models. Technology can be a real ally in doing so.
1.2 The health network: a patient‑centered and preventive vision
A health network goes beyond purely clinical care. It includes:
- Prevention and health promotion,
- Data analysis to identify risks,
- Collaboration between healthcare, social services and related fields,
- The ability to influence health determinants (lifestyle, environment, psychological factors),
- Technology as a central infrastructure.
Switzerland does not just need better care organization: it needs a system capable of anticipating, preventing and coordinating at a larger scale.
2. Three major challenges of the Swiss health system
2.1 Shortage of qualified staff and administrative overload
The shortage of qualified personnel is one of the central challenges of the Swiss health system today. Many institutions lack nurses, assistants and even doctors, especially in family medicine. Some striking figures:
- One in four doctors is 60 or older in Switzerland and will be nearing retirement in the coming years
- Four in ten nurses leave the profession early, a third of them before age 35
- Two in ten community care assistants abandon their profession within five years of graduation
Planète Santé describes a “deep malaise” and points out that burnout is not just about working conditions, but also a loss of meaning: caregivers are caught between patient care and profitability logic and are therefore subject to “paradoxical injunctions,” according to Bertrand Kiefer, editor‑in‑chief of the Swiss Medical Journal. This phenomenon makes the transition from a care network to a health network essential, where prevention, coordination, standardized procedures and digital tools reduce non‑clinical burden.
2.2 Aging population and chronic diseases
Furthermore, Switzerland is aging. Demographic projections show a rapid increase in the proportion of older people, often suffering from multiple chronic diseases at once. In this context, prevention, early detection and the ability to organize continuous care pathways become essential: chronic disease monitoring, collaboration with nursing homes and home care services, etc. Here too, the importance of prevention to avoid overloading the care system is essential.
2.3 Healthcare costs under strong pressure
Health insurance, hospitalizations, long‑term care: the overall bill continues to rise. Both PNR 74 and Deloitte emphasize that the Swiss system must respond to growing needs while containing already very high costs. A key issue is that interprofessional coordination, although central in care networks, is still poorly or insufficiently valued in financing models. Time spent discussing cases, preparing hospital discharges or harmonizing treatment plans is rarely compensated at its true worth.
3. Main solution areas for a more effective health network
In the face of these challenges, shifting from a care network to a health network puts the patient back at the center of their care journey. To achieve this, solutions must be organizational, financial and cultural. Technology can help make them concrete, measurable and sustainable over time.
3.1 Integrated care and coordination: putting the patient first
One of the key challenges of the health network, as mentioned above, is the need to better coordinate care, especially for people with chronic conditions. In Switzerland, this effort involves:
- Strengthening regional health networks and models like managed care (with GP lists, initial video consultations, etc.)
- Developing health centers or group practices with interprofessional teams
- Better recognition of coordination in reimbursement models
To function daily, these models need tools that simplify information sharing, such as the electronic patient record (soon to be the electronic health record), appointment planning, referrals to the right professionals, and care protocol management.
3.2 Prevention and public health: reducing avoidable demand
The 2025–2028 Strategy of Health Promotion Switzerland focuses on health promotion and prevention, particularly regarding non-communicable diseases, mental health and social determinants of health. Investing in prevention means:
- Reducing the progression of certain chronic diseases
- Delaying loss of autonomy
- Reducing pressure on emergency departments, hospital stays and long-term care
Here, digital tools can play a key role: screening reminders, targeted prevention programs, remote monitoring, etc. Deloitte estimates that if the system focused more on prevention and digitalization, healthcare costs could be reduced by CHF 30 billion by 2040. Our survey conducted with MIS Trend and Farner confirmed this: over half of respondents believe AI could help reduce healthcare costs.
3.3 Funding reforms: creating the right incentives
Discussions on the 2nd revision of the LAMal, new tariffs (like TARDOC) or network-based insurance models aim to:
- Better compensate outpatient services
- Reduce misaligned financial incentives favoring hospital stays
- Encourage integrated care and coordination models
These reforms rely on improved quality measurement, resource use and patient outcomes — which require reliable data and adapted information systems.
3.4 Digital solutions: a key lever to cut costs and reduce admin workload
Digital isn’t an end in itself. But it becomes a major driver when building health networks in Switzerland. In practical terms, several solutions can ease the burden on the system, professionals and patients alike:
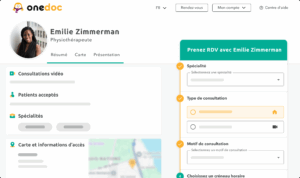
- Online appointment booking improves patient experience while reducing secretarial tasks. No more phone tag or reminder calls — everything is handled automatically via SMS reminders and confirmation emails.
- The electronic patient record (soon the electronic health record) centralizes patient data in one place and avoids duplicate exams or complex health data transfers. These tools are often designed to integrate directly into your medical software.
3.5 Teleconsultation: relieving the system through remote care
Another way to ease the burden on the healthcare system is through telemedicine. Though promoted in some insurance models, it’s not yet widespread in Switzerland. Yet teleconsultation is well-suited for minor health issues when in-person care isn’t necessary. In practical terms, for a follow-up visit or prescription renewal, telemedicine can save time — time that can be spent on patients with greater needs.
3.6 AI: a partner in health networks?
Many doctors and therapists wonder whether artificial intelligence will eventually replace them. But studies offer reassuring insights: AI is more of a support tool than a replacement for healthcare professionals. And Swiss patients agree: our study found that only 2% completely trust AI for medical diagnoses. Still, AI can be a powerful ally in healthcare:
- Assists with image analysis (radiology, dermatology, ophthalmology, etc.) by detecting patterns the human eye might miss
- Helps triage incoming requests: prioritizing messages, routing patients to the right professional
- Supports drafting reports or standard letters for doctor review
- Identifies weak signals needing follow-up or screening, based on structured data
Toward a sustainable health network through technology?
Switzerland’s healthcare system faces structural challenges: a shortage of qualified staff, an aging population, rising chronic disease, growing cost pressures… The shift from a care network to a health network is essential to meet these demands. Combined with technology, this paradigm shift should reduce admin burden, streamline care pathways and strengthen interprofessional collaboration. Solutions like OneDoc support exactly this approach: offering simple, practical tools that integrate with your workflow — so you can spend more time on what matters most: caring for your patients.