In a dermatology practice, emergencies are part of daily life: skin infections, allergic reactions, post-surgical complications. But when they’re not anticipated, they can quickly throw off your schedule, cause delays, and increase pressure on your entire team.
The good news: practices that manage dermatological emergencies without disrupting the day implement a few simple methods that you can adopt today.
How emergencies often disrupt dermatology practices
Managing medical emergencies is a challenge for many practices — especially in dermatology, where the line between a true emergency and a perceived emergency is sometimes blurry. But the issue isn’t the emergency itself — it’s the lack of a clear framework in how the practice is organized.
Indeed, if nothing is set up to anticipate emergencies, you can quickly face cascading delays, overload for your medical staff, and a worsening of the patient experience
3 Methods to effectively anticipate dermatological emergencies
Managing medical emergencies is a challenge for many practices — especially in dermatology, where the line between a true emergency and a perceived emergency is sometimes blurry. But the issue isn’t the emergency itself — it’s the lack of a clear framework in how the practice is organized.
Indeed, if nothing is set up to anticipate emergencies, you can quickly face cascading delays, overload for your medical staff, and a worsening of the patient experience
1. Prioritize by type of dermatological emergency
In dermatology, some situations require fast intervention. The key question is always: which emergencies need a quick check, and which can wait?
Medical triage in dermatology allows you to distinguish:
- True medical emergencies (severe infections, post-surgical complications)
- Functional or aesthetic urgencies
- Non-urgent requests perceived as urgent by the patient
Without this triage, your schedule quickly becomes unmanageable, and patient flow becomes unbalanced. That’s why we recommend setting up a triage system before consultations.
Triage methods in dermatology
Remotely: Before triaging patients in your office, you can ask them to send a photo of their skin issue or schedule short teleconsultations. This helps you decide which patients need urgent care.
In the office: You can implement several methods to keep your practice organized during emergencies. A common approach is using a triage matrix adapted to dermatological needs. Here’s one you can tailor to your setup:
| Priority level | Examples | Recommended timeframe | Organizational action |
|---|---|---|---|
| Level 1: Immediate emergency | Acute skin infection (abscess, cellulitis, erysipelas), post-surgical complication (bleeding, intense pain, signs of infection), severe or widespread allergic reaction, suspected skin necrosis | Same day | Fit into an urgent buffer slot or create a dedicated slot |
| Level 2: Relative emergency | Significant but stable skin inflammation, rapid worsening of a known lesion, suspected early infection, post-treatment reaction without severe symptoms | 24 to 72 hours | Priority appointment or preliminary evaluation (photo or teleconsultation) |
| Level 3: Non-urgent perceived as urgent | Chronic lesion with no recent change, stable aesthetic issue, follow-up without acute symptoms, mild chronic itching | Standard availability | Schedule as a regular appointment with clear information and reassurance |
2. Plan dedicated buffer slots
Optimizing your medical schedule is all about anticipation.
The most well-organized practices intentionally include buffer slots throughout the day to absorb emergencies without disrupting the entire agenda.
These slots can be used for:
- An emergency consultation
- An unplanned post-surgical follow-up
- Making up for a slight delay
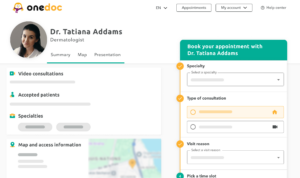
If you’re using an online appointment booking tool, you can choose to restrict certain types of appointments to specific time slots. This makes it easy to reserve buffer times.
3. Adjust appointment durations
Not all dermatology consultations take the same amount of time. Take the time upfront to configure your appointment types in your medical software and define the actual duration of each visit to avoid unexpected issues.
Start by identifying and grouping your appointment types into consistent categories such as:
- First consultation
- Check-up/follow-up
- Dermatological emergency
Once each group is defined, make sure each category has a realistic duration based on your daily practice, not just theoretical estimates. This is especially important for treatment protocols where multiple people, materials, and rooms may be involved.
Finally, make sure these appointment types are clear to your team—and to your patients. This helps keep your schedule easier for everyone to follow.
The case of dermatological surgery
Dermatological surgery requires even more rigorous organization. Post-operative emergencies often need to be handled quickly—without disrupting your scheduled consultations.
Managing emergencies without being overwhelmed: a win for your practice and your patients
Dermatological emergencies aren’t an anomaly—they’re a reality that should be fully integrated into your workflow. When properly anticipated, they no longer throw off your day and instead blend naturally into your schedule. The key lies in a balanced combination of pre-consultation triage, smart time management, and tools tailored to dermatology.
With these methods, your goal isn’t to eliminate emergencies—but to handle them without letting them disrupt your day. That way, you can keep your schedule on track, reduce pressure on your team, and offer a better experience to all your patients—emergency or not.