Artificial intelligence in medicine is no longer a distant promise; it is now part of the daily routine of many healthcare professionals in Switzerland. From hospitals to medical practices, medical AI technologies are gradually being integrated into clinical, diagnostic and administrative workflows.
But where does AI in the Swiss healthcare sector stand today? This is exactly what we aim to explore in this article. From concrete applications and benefits for physicians to its limitations, risks, and the ethical and regulatory challenges specific to the Swiss healthcare system.
What is meant by artificial intelligence in medicine?
Let us start by defining the basics: artificial intelligence in healthcare refers to all computer systems capable of learning from medical data and producing analyses, predictions or recommendations. These systems are primarily based on machine learning and deep learning, meaning that the machine can independently understand and learn from the data provided to it.
In practical terms today, AI can:
- Analyse medical images (MRI, CT scans, X-rays)
- Process complex clinical and biological data
- Identify patterns invisible to the human eye
- Calculate probabilities of risk or clinical progression
Key point: AI systems do not make diagnoses autonomously. They provide indications that are interpreted and validated by the physician.
Current use cases of AI in medicine in Switzerland
The adoption of AI in medicine is progressing pragmatically. In Switzerland, several fields already stand out through concrete applications.
Medical imaging diagnostics
AI is widely used to support medical diagnosis. It is also one of the most extensively studied fields internationally. In practice, it analyses:
- Medical images
- Biological signals (ECG, EEG)
- Laboratory data and patient records
More specifically, it is used in the following specialties:
- Radiology (MRI, CT scans, X-rays)
- Dermatology (analysis of skin lesions)
- Pathology (histological slides)
Artificial intelligence is particularly effective here in detecting abnormalities and patterns early in the care pathway. Human validation remains essential.
Prediction and early warning systems
In hospital departments, AI is used to:
- Continuously monitor vital parameters
- Detect clinical deterioration at an early stage
- Anticipate events such as epileptic seizures or organ failure
These models continuously analyse vital parameters and can, for example, alert clinicians in advance of a heart attack or stroke.
Personalised therapies and oncology
AI increasingly supports individualised therapeutic strategies:
- Analysis of real-world data and registries
- Therapeutic decision support in oncology
- Combination of imaging, genomic and clinical data
The goal is to adapt treatments to the individual patient profile based on comparable cases.
Medical research and drug development
In Swiss research centres and university hospitals, AI enables:
- Faster identification of promising molecules
- Efficient analysis of large clinical data sets
- Improved understanding of certain disease mechanisms
Reduction of administrative burden
AI in the medical field is not limited to direct patient care. It also plays a key role in the daily work of physicians and assistants:
- Automatic transcription
- Support in drafting reports, letters and clinical summaries
- Support in managing patient flows
- Reduction of repetitive tasks that can be automated
- Chatbots to help guide patients
The benefits of AI in healthcare for physicians
As we have seen, when properly integrated, AI offers concrete benefits in the medical field:
- Faster and more sensitive detection of certain diseases
- Reduction of the workload related to repetitive tasks
- Time savings that can be used for complex cases and patient communication
- Support for personalised therapeutic decisions
- Improvement of prognostic models
- Support for medical research
In a context of staff shortages and increasing pressure on healthcare systems, these advantages are particularly significant.
Limitations and risks of AI in medicine
Despite its potential, AI also presents important limitations, making the role of healthcare professionals even more essential.
Medical data quality and bias
The performance of AI depends heavily on training data. These data may not be representative and can introduce bias. For example, the population represented in the training data may differ from the population benefiting from AI-based diagnostics.
Many models are also trained outside Europe, which limits their transferability to the Swiss context and can raise questions about the origin and use of the data.
Another limitation is that data quality may be poor or data may not be correctly labelled, preventing AI systems from drawing reliable conclusions and potentially leading to unusable results.
This is compounded by overfitting to training data, where a model fails to make accurate predictions once new data diverge from the training set.
Finally, in rare or novel situations, AI systems tend to show reduced performance or may not know how to proceed appropriately.
Lack of transparency
Since AI models generally learn “on their own” from the data provided to them, it is often not possible to understand exactly how they operate. These models thus become true “black boxes”, which can hinder clinical trust.
Ethical challenges and legal framework in Switzerland
In Switzerland, the use of AI in medicine is governed by:
- The revised Federal Act on Data Protection (nFADP)
- Swissmedic requirements for medical devices
- Recommendations from the FMH
Key principles include in particular patient data protection, transparency and traceability, fairness and non-discrimination, as well as patient safety.
As discussed above, some of these principles are not always fully compatible with the current limitations of AI.
This raises an important question: in the event of an error, who is responsible – the AI or the physician?
At present, the position is clear: the physician remains responsible for all clinical decisions.
What impact does AI have on the medical profession?
As shown throughout all sections on the application of AI in healthcare, healthcare professionals remain at the centre of the Swiss care system. To the question of whether AI will replace physicians, the answer is clear: no. AI is not intended to replace doctors; it should be viewed as a tool. Physicians remain essential for analysing data, interpreting recommendations and making clinical decisions.
AI primarily helps to free up time for what matters most: the patient relationship, communication and complex decision-making.
The future of AI in medicine in Switzerland
Looking at recent developments in AI in Switzerland, upcoming advances will notably include:
- Multimodal models capable of combining images, text and sensor data
- More predictive tools for prevention
- The rise of generative AI for medical documentation and knowledge management
- Patients arriving better informed at consultations after using chatbots such as ChatGPT
Summary: Applications of AI in medicine
| Area | Examples of applications |
|---|---|
| Diagnosis | Image analysis, risk scores |
| Therapy | Decision support, personalisation |
| Research | Drug development |
| Organisation | Appointment management, resources |
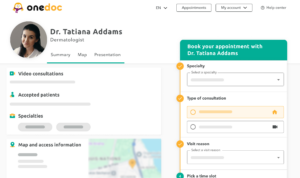
| Communication | Chatbots, telemedicine |
AI in medicine: a promising technology with limitations
Artificial intelligence in Swiss medicine opens up major opportunities to improve the quality of care and reduce the workload of physicians. Its adoption should, however, remain gradual, well regulated and centred on human values.
When used responsibly, AI becomes a valuable ally for physicians, serving a more efficient and sustainable Swiss healthcare system.
FAQ – AI in medicine
Are physicians already using AI in Switzerland?
Yes, particularly in radiology, medical imaging and the organisation of medical practices.
Can AI make a diagnosis?
No. It analyses images and clinical parameters to identify relevant patterns and provides indications, but the final decision always lies with the physician.
What are the main benefits of AI in medicine?
AI in medicine helps in particular to save time, improve early detection and support data-driven decision-making.
What are the risks?
Algorithmic bias, lack of transparency, data protection issues and questions of liability.
Will AI replace physicians?
No. It complements human expertise rather than replacing it.